The COVID-19 pandemic has profoundly impacted mental health globally, with the UK experiencing a significant surge in mental health challenges.
As lockdowns, social isolation, and economic stress took their toll, mental health services across the country faced unprecedented demand.
Statistics on Mental Health Service Usage Post-Pandemic
This article examines the rise in mental health service usage post-pandemic, exploring key statistics, regional trends, and barriers to care while offering insights into the policies and solutions required to address these challenges.
Overview of Mental Health Challenges Post-Pandemic
Globally, the World Health Organization (WHO) reported an increase of over 25% in anxiety and depression cases during the pandemic.
In the UK, these challenges were magnified by prolonged lockdowns, economic uncertainty, and a strained healthcare system. Data from NHS England highlights a surge in demand for mental health services, with referrals reaching all-time highs post-pandemic.
The Mental Health Foundation reported that 1 in 4 adults experienced significant mental health struggles in 2022, compared to 1 in 6 pre-pandemic, reflecting the long-lasting impact of the crisis.
Key Statistics on Mental Health Service Usage
Usage Trends
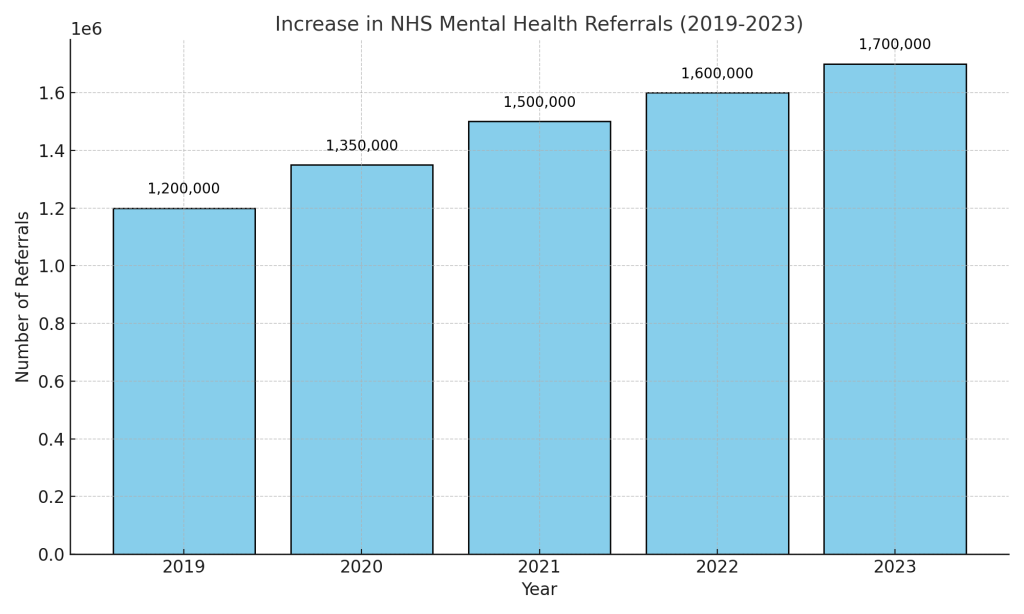
- NHS mental health referrals increased by 25% in 2021 compared to pre-pandemic levels, according to NHS Digital.
- By 2022, over 1.6 million individuals were actively in contact with mental health services in England.
Demographics

- Children and young people saw the highest increase, with referrals rising by 35% post-pandemic.
- Adults aged 18-34 reported the highest prevalence of anxiety-related conditions, according to the Office for National Statistics (ONS).
Regional Insights
- Urban areas like London and Manchester experienced the highest demand for services.
- Rural regions reported limited access to care, exacerbating disparities in service delivery.
Barriers to Accessing Mental Health Services
Despite increased demand, accessing mental health services remains a challenge for many:
Staff Shortages
The Royal College of Psychiatrists reported a 10% shortfall in qualified mental health professionals, leaving many services understaffed.
Waiting Times
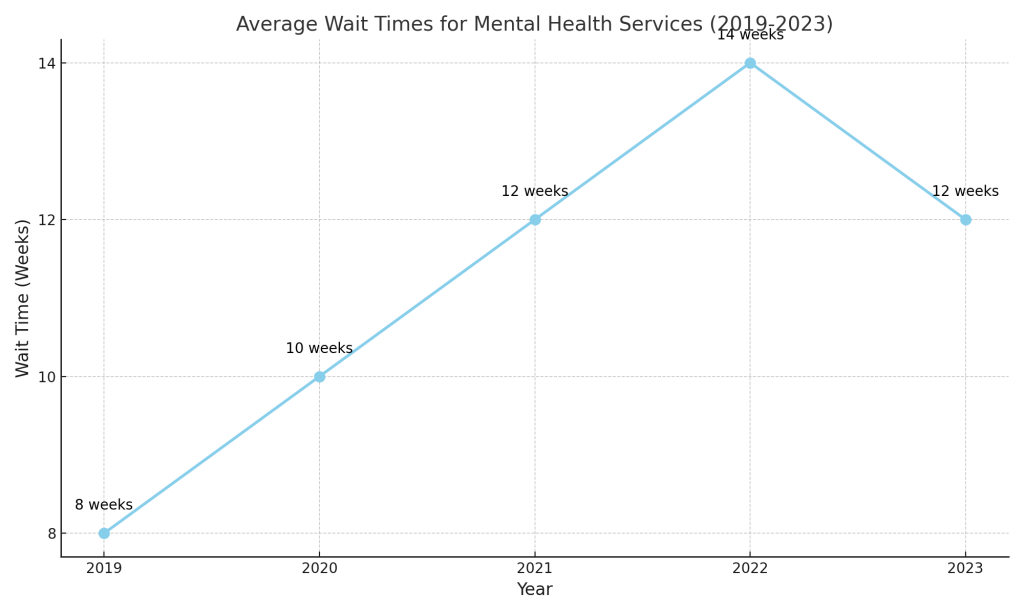
Average wait times for NHS mental health services increased to 12 weeks post-pandemic, with some regions experiencing even longer delays.
Geographical Disparities
Rural areas face a lack of adequate mental health facilities compared to urban regions, further limiting access to care for vulnerable populations.
Impact of Increased Service Usage
Positive Outcomes
- The expansion of telehealth services post-pandemic allowed more people to access mental health support remotely.
- Increased awareness and destigmatization of mental health issues have led to more individuals seeking help.
Challenges
- The surge in demand has strained existing services, leading to longer wait times and increased burnout among mental health professionals.
- Rising costs of private therapy have created affordability barriers, particularly for low-income households.
Policy Implications and Solutions
Government Initiatives
- The NHS Long-Term Plan aims to improve mental health services by 2024, with a focus on expanding access for children and young people.
- The UK government allocated additional funding to bolster mental health services, including initiatives to train new professionals.
Recommended Solutions
- Training and Retention: Investing in the recruitment and retention of mental health professionals to address staff shortages.
- Telehealth Expansion: Building robust telehealth infrastructure to reduce waiting times and extend services to underserved areas.
- Targeted Interventions: Addressing high-risk demographics, such as children and young people, through targeted mental health programs.
Conclusion
The post-pandemic surge in mental health service usage highlights the urgent need for a sustained focus on improving mental health care in the UK. From addressing staffing shortages to expanding telehealth, solutions must prioritize accessibility, affordability, and equity. As the UK navigates the aftermath of the pandemic, these efforts will be essential in ensuring the mental wellbeing of all its citizens.